The physical principles behind Bioelectrical Impedance Analysis (BIA) technology have been established for decades, but every newly developed body composition analyzer must still answer the same question that might keep engineers awake at night: Are the measurements accurate?
Correct technical principles don′t guarantee reliable implementation. It′s like knowing you need high heat to sear a steak and lock in the juices—that doesn′t mean what comes off your pan won′t resemble a hockey puck. How the electrodes are designed, what frequencies are used for measurement, how the algorithms are calibrated, applicability across different ethnicities and body types... these subtle differences ultimately leave their mark on measurement quality. This is why clinical validation is so important. It uses real human bodies, real-world usage scenarios, and rigorous statistical methods to prove that a device isn′t just "theoretically sound," but actually "measures accurately in practice."
We conducted a clinical validation study using STARBIA MEDiTEK′s portable body composition analyzer STARBIA201 (hereafter referred to as SA201), recruiting a total of 177 healthy Taiwanese adults aged 25 to 86, including 55 men and 122 women. Their Body Mass Index (BMI) ranged from 13.52 to 39.59 kg/m², covering virtually every body type from underweight (seriously, are you eating enough?) to obese (maybe time to reconsider that daily bubble tea habit?). Each participant was measured by three instruments: STARBIA MEDiTEK′s SA201, the well-known InBody770, and DXA (Dual-energy X-ray Absorptiometry), the gold standard for body composition in the medical field. We then compared the measurement results from all three.
First, we compared the measurements of total body water, intracellular water, extracellular water, abdominal visceral fat area, and basal metabolic rate obtained by SA201 and InBody770. We used Pearson′s correlation coefficient to assess whether the results from the two instruments were consistent.
Pearson′s correlation coefficient, represented by r, ranges from -1 to 1. It′s suitable for describing the relationship between two continuous variables. In this study, we used it to evaluate the consistency between the two instruments′ measurements.r = 1 represents perfect positive correlation—the two instruments′ measurements move in perfect lockstep, basically twin telepathy levels of agreement; r = -1 represents perfect negative correlation, meaning the two instruments contradict each other at every turn, with measurements showing completely opposite trends; r = 0 means no relationship whatsoever. The closer the correlation coefficient is to 1, the more consistent the measurements between the two instruments.
The results showed correlation coefficients of 0.99 for total body water, intracellular water, abdominal visceral fat area, and basal metabolic rate, with extracellular water achieving 0.98. In plain English: the results measured by the two instruments were virtually identical. These numbers are so good you could frame them and hang them on your wall.
Next, we compared SA201 and DXA measurements of body fat percentage, lower limb muscle mass, appendicular skeletal muscle mass, appendicular skeletal muscle mass index, total body bone mineral content, and total body bone density.
DXA (Dual-energy X-ray Absorptiometry) uses two X-ray beams of different energies to penetrate the human body, distinguishing body composition based on how different tissues absorb X-rays. Bone has the highest density and absorbs the most X-rays; fat tissue is next; muscle and other lean tissues absorb less. By comparing the transmission rate differences between the two energy X-rays, DXA can calculate the mass and distribution of these three tissue types, with small measurement errors and low variability in repeated measurements.DXA was originally developed to measure bone density and diagnose osteoporosis, and has been used in clinical medicine for decades, accumulating substantial research data and practical experience. Researchers later discovered it could also precisely measure body composition, gradually becoming the reference standard for body composition research. To put it in perspective, DXA is basically the black belt master of the body composition measurement world—if you want to prove your device′s capabilities, you need to go toe-to-toe with the reigning champion.

AI generated image
The results showed that SA201 and DXA demonstrated high correlations across all indicators, including body fat percentage (r = 0.92), lower limb muscle mass (r = 0.96), appendicular skeletal muscle mass (r = 0.97), appendicular skeletal muscle mass index (r = 0.93), bone mineral content (r = 0.88), and bone density (r = 0.81). This means that when DXA detects high body fat in someone, SA201 yields corresponding results; when DXA shows someone has abundant muscle mass, SA201 detects the same. In other words, although SA201 and DXA use completely different technical principles to measure body composition (SA201 relies on electrical resistance, DXA relies on X-rays), they′re measuring the same physiological reality.
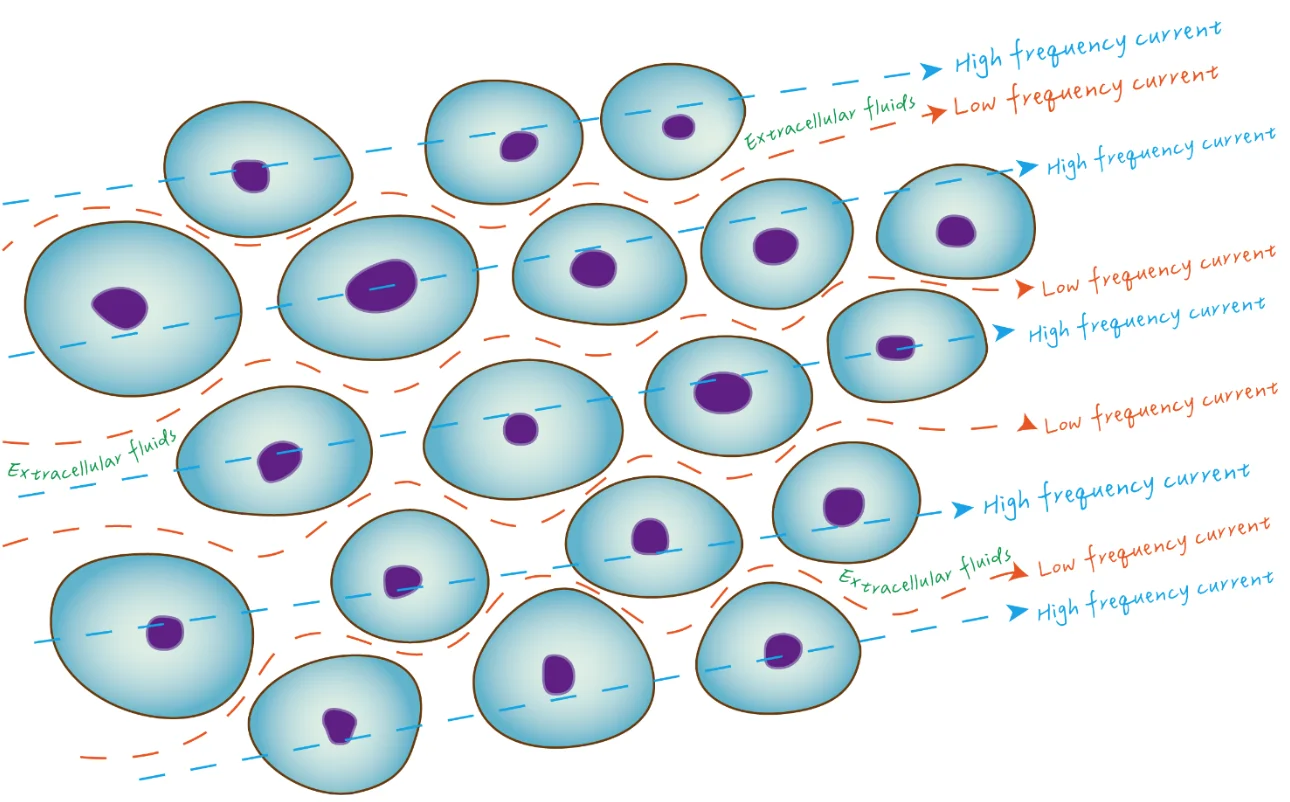
Why were intracellular water, extracellular water, and total body water only compared with InBody and not with DXA? You might wonder: why were intracellular water, extracellular water, and total body water only compared with InBody and not with DXA? Is DXA being difficult? Not at all. DXA′s measurement principle uses X-rays of different energies to penetrate human tissue, distinguishing between bone, fat, and lean tissue based on tissue density differences. While DXA can precisely measure the mass and distribution of these three major tissue categories, it cannot further separate water and protein within lean tissue, much less distinguish between intracellular and extracellular water. It′s like having a bathroom scale that can tell you your suitcase weighs 50 pounds, but can′t tell you how many shirts, shoes, or toiletries are packed inside. Not a knock on the scale—it′s just not designed for that level of detail. In contrast, water measurement is at the core of BIA technology. Electrical current conduction in the human body primarily depends on electrolytes in body fluids. Low-frequency current cannot penetrate cell membranes and can only conduct through extracellular fluid; high-frequency current can penetrate cell membranes and conduct through both intracellular and extracellular fluid. By utilizing the impedance differences caused by different frequency currents, BIA devices can first estimate total body water, then calculate extracellular water based on low-frequency current impedance, and finally derive intracellular water by subtracting extracellular water from total body water. Therefore, when validating SA201′s water measurement function, we compared it with InBody770, a professional device that also uses BIA technology and has been thoroughly validated. To benchmark water measurements, you need to compare apples to apples.
The physical foundation of BIA technology has long been established, but each new device must still prove: electrodes are positioned correctly, measurement frequencies are appropriately selected, algorithms are properly calibrated, and accurate results are obtained with real users.
The study results show that SA201 not only aligns with reference devices in "trend of change," but also achieves excellent agreement in "absolute values." This means it can be used not just to "track changes" (such as whether body fat decreases during a cutting phase), but also to provide "absolute assessment" (such as whether current muscle mass is adequate). This study was conducted in Taiwan, validating SA201′s reliability for measurements on Asian populations.
Of course, even the most accurate instrument can′t stop you from hitting up the fried chicken joint after work. But at least when you step on the SA201, it will honestly tell you: your body remembers every single one of those late-night snacks from last week.